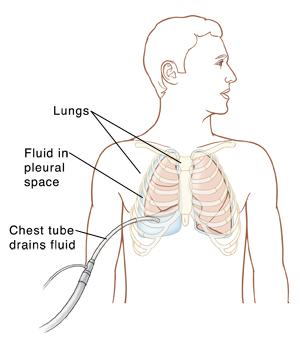
Chest Tubes
Your lungs are each surrounded by two layers of membrane (pleura). The space between these layers is called the pleural space. Normally the pleural space has a tiny amount of fluid in it. But extra fluid, blood, pus, or air in the pleural space makes it hard for the lung to expand and makes breathing hard. A chest tube is a soft, flexible tube put into the pleural space that surrounds the lung. The tube doesn't go into the lung itself. The tube drains blood, air, or extra fluid. The tube is inserted through a small cut (incision) in the skin.
Reasons for a chest tube
You may need a chest tube:
-
After chest surgery or injury to the chest
-
To treat a lung infection or abscess. This is called an empyema.
-
To remove extra fluid from around the lung from other causes. This is called a pleural effusion. This might be from heart failure.
-
To treat collapsed lung (pneumothorax)
-
To treat bleeding into the chest (hemothorax)
Chest tube placement
A chest tube is often placed during chest surgery while you’re in the operating room and still asleep (sedated). If you have a lung infection or other problem, you may have a chest tube placed while you’re awake in the emergency department,your hospital room, or in a radiology suite. The procedure takes less than 30 minutes. Here’s how it's done:
-
Medical staff takes your blood pressure, pulse, and temperature.
-
You lie on your side or sit in a semi-upright position. You will be asked to put one arm up over your head.
-
The healthcare provider injects pain medicine (anesthetic) to numb the area where the chest tube is placed. You may be given medicine to make you relax (sedation) or pain medicine. Sedation is given in an IV (intravenous) line in your hand or arm.
-
The provider makes a small incision in your side, chest, or back. They put a soft, flexible tube into the incision site. The tube is guided between your ribs until it reaches the pleural space. The provider may use ultrasound imaging or computed tomography (CT) to help place the tube correctly.
-
The provider may stitch the tube to your skin to keep it in place. It will also be covered with an airtight bandage. The tubing will be taped to your body. This is to keep it from being pulled out by accident.
-
The tube is then connected to a drainage device.
-
A chest drainage unit pulls the extra fluid, blood, pus, or air from your chest. The device should be lower than your chest level and may be put on the floor. Some chest tubes contain water and may make a bubbling sound while they are working. Other chest tubes will not make any sound at all.
-
A flutter valve is a small one-way valve. It's used if you have a collapsed lung ( pneumothorax). The lung collapsed because of the collection of air in the pleural space. The valve is attached directly to the end of your chest tube. The valve opens to let air escape from the chest tube. It then closes to prevent air from going back in the tube. You may go home from the hospital with your chest tube attached to a flutter valve. Care for it as you are told.
-
You will have an X-ray after the procedure to help confirm that the tube is in the right place, and that the air and fluid have been drained.
While the tube is in place
-
The tube stays in place for as long as your healthcare provider thinks it's needed. You may be in the hospital until after the tube is removed. Sometimes you may be sent home with the chest tube still in place. If you are sent home with the chest tube in place, you will need home healthcare or a caregiver until it is removed.
-
You will be given pain medicine by mouth or by IV. You may have a patient-controlled analgesia (PCA) pump attached to the IV line. This lets you give yourself pain medicine, but it's programmed so you can't overdose. You are usually sent home when you can take oral pain medicine and no longer need IV pain medicine.
-
You may need extra oxygen. This is given through a mouth mask or a flexible tube under your nose. You may also be connected to a small device called a pulse oximeter. It measures the amount of oxygen in your blood. It is placed on your finger, toe, or ear.
-
After the tube is placed, you can help with drainage by:
-
You can reduce discomfort by holding a pillow tightly to your chest when you cough.
-
Your breathing and heart rate will be monitored. The tubing will be checked regularly. If blood is draining from your chest, the tubing will be checked for clots. If a clot appears, the tubing may be squeezed to move the clot out of the tube. If fluid is draining from your chest, it may be tested for signs of infection or other problems. You may need antibiotics to prevent or treat infection.
-
Tell a nurse right away if you have trouble breathing or chest, shoulder, or neck pain.
Risks and possible complications of chest tubes
A chest tube can have some risks. But the benefits of having the tube usually outweigh the risks. Risks of a chest tube include:
Caution!
Don't pull on the tube or tip over the drainage container. This can cause serious breathing problems. If you pull on the tube or tip over the container, tell a nurse right away. You may be asked to exhale fully or take deep breaths while the tubing is checked.
Removing the chest tube
When the air, blood, pus, or extra fluid is gone from the pleural space, your healthcare provider will remove the tube. This may be done in your hospital bed. You may get more pain medicine before the tube is removed. As the tube is removed, you may be asked to inhale or exhale deeply and then hold your breath. After the tube is removed, the healthcare provider may close the incision with stitches. Or the incision may be left to close by itself. The provider will put a bandage over the incision. You may have an X-ray after the tube is removed. This is to make sure your lung is still inflated.
Follow-up care
After the tube is removed:
-
Follow up with the healthcare provider within 48 hours. You may have another X-ray. This is to check for fluid or air in your lung. The incision will be checked to make sure it's healing. The bandage may be replaced with a smaller adhesive bandage. You may change the bandage as often as needed.
-
Care for the insertion site(s) as directed. Keep the bandage in place for 48 hours. Keep it dry.
-
Until a scab has formed on the incision site, you may shower but not take a bath. When a scab has formed, you no longer need an adhesive bandage. After the incision has healed, you may have a small scar.
When to call the healthcare provider
While the tube is in place and after it has been removed, call 911 oryour healthcare provider (or alert your nurse) right away if you have any of the following:
Call 911 if you have any of these:
Call your healthcare provider if you have any of these:
-
Fever of 100.4ºF (38ºF) or higher, chills, or as directed by your healthcare provider
-
Weakness or dizziness
-
Increasing pain, swelling, redness, warmth, bleeding, foul odor, or drainage at the chest tube site