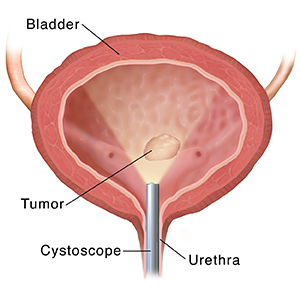
Treating Bladder Cancer: Transurethral Resection (TUR)
Cystoscopy is a procedure your healthcare provider uses to look at the inside of your bladder and urethra. The urethra is the tube that connects the bladder to the outside of the body. For a cystoscopy, a thin tube with a tiny camera on it is passed through your urethra and into your bladder. This tube is called a cystoscope or resectoscope. Problems in the urinary tract can be found and sometimes even treated during a cystoscopy.
If cancer is found and it's in an early stage (small) and is growing slowly (low grade), it may be taken out during cystoscopy. This is called a trans urethral resection (TUR) or trans urethral resection of bladder tumor (TURBT). The surgery to remove the tumor is done through the scope. No cut is made in your skin. TUR can be used to diagnose or treat bladder cancer.
Most of the time, the tissue taken out during TUR is checked under a microscope at a lab. This is done to see exactly what it is and if more treatment is needed.
Before cystoscopy
TUR is most often done in a surgery center or hospital as an outpatient procedure. So you can often go home the same day. If the tumor is large, you might stay overnight.
You'll be given medicine so you don’t feel pain during the procedure. This is called anesthesia. If you have regional anesthesia, just the lower part of your body is numbed. Medicine may also be used to make you feel sleepy. If you have general anesthesia, you'll be in a deep sleep during the procedure.
During the procedure
A cystoscope or resectoscope is passed through your urethra and into your bladder. The lining of the bladder is looked at through the scope. If tumors are found, they're taken out if possible. A wire-like cutting tool in the scope is used to do this. After the tumor is removed, electrocauterization might be used to seal off blood vessels. This is done to prevent bleeding.
A sample of cells (biopsy) from the tumor and normal-looking tissue may be taken out. These samples are checked under a microscope in a lab. This is done to look for cancer and, if it's found, to see how deeply it has grown into the bladder wall. In some cases, a laser is then used to burn any remaining tumor away.
After the procedure
Here is what to expect after TUR:
-
After the procedure, a thin, flexible tube (called a catheter) might be put in your bladder. It drains pee and blood out of your bladder while you heal. The tube may be in for a few days. There may be blood in your pee for a few weeks.
-
Bladder tumors can come back (recur) after treatment. To be sure that all cancer cells are killed, TUR may be followed by other types of treatment. This may include intravesical therapy. This is when medicines are put into the bladder to kill the cancer cells.
-
TUR might be done again if the biopsy shows that all the cancer cells weren't taken out. The TUR will make sure all of the cancer is removed. Or it will take a deeper biopsy to check for cancer.
Risks and possible complications of TUR
All procedures have risks. Risks of TUR include:
-
Blood or blood clots in your pee
-
Bladder spasms and irritation
-
Pain when peeing
-
Having to pee more often than normal (urinary frequency)
-
Trouble controlling your pee
-
Urinary tract infection
Most of these go away on their own or can be treated. They don't last very long.
If TUR is repeated many times, it can cause scarring. And the bladder may not be able to hold much pee. This can lead to needing to pee often (urinary frequency) and trouble controlling your pee (incontinence).
Working with your healthcare provider
Your provider will talk with you about TUR and answer any questions you may have. They'll help you understand why it's being done, what it will be like, and how you may feel during and after TUR. Be sure you know what problems to watch for and when you need to call your provider. Or when to get medical care right away. Also be sure you know what number to call to get help after office hours, on weekends, and on holidays.